What are Epileptic seizures?
Our brain cells speak to one another with electrical signals. Epileptic seizures arise as a result of disturbances in brain cells’ electrical activity. Our brain controls every functions of our body, hence epileptic seizures can manifest in many ways. Children who experienced epileptic seizures might lose their consciousness, or they might have strange sensations or feelings, or movements they can’t control. They might ever go stiff or floppy, fall to the floor and shake.
What Are the Types of Epileptic Seizures?
In general, epileptic seizures can be divided into generalised onset or focal onset epileptic seizures. ‘Generalised epileptic seizures’ appear to start from both sides of the brain simultaneously, whereas, ‘focal epileptic seizures’ start from a specific area of the brain.
Epileptic seizure can also start from one area of the brain and then spread to both sides of the brain, and this is called ‘focal to bilateral tonic clonic seizure’.
There are many types of ‘General epileptic seizures’ and ‘Focal epileptic seizures’. The followings are the common types:
| Generalised Epileptic Seizures | Focal Epileptic Seizures | ||
|---|---|---|---|
|
|
What is Epilepsy?
Epilepsy is a group of disorders in which recurrent epileptic seizures occur. Up to 5% of human beings will have at least one epileptic seizure in their life-time; and not all of them will develop recurrent epileptic seizures or epilepsy.
Epilepsy can start at any age, and there are many different types of epilepsy. Approximately 1 in 200 children and young people have a diagnosis of epilepsy. However, it is important to know that epilepsy is not necessary a life-long condition.
The misdiagnosis rate of epilepsy is high. Up to 30% of children may be diagnosed with epilepsy when they do not have epilepsy; and those who have epilepsy may be left without an appropriate diagnosis.
What Types of Epilepsy are there?
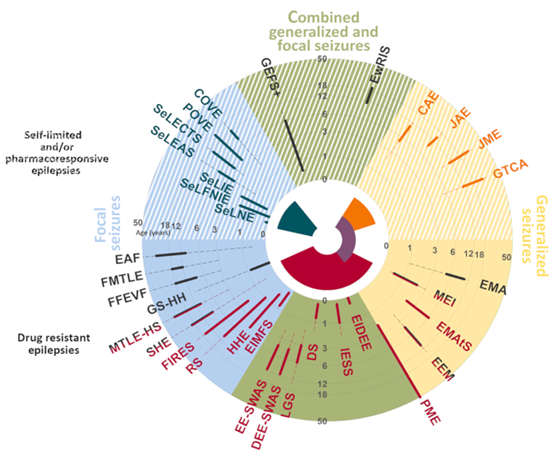
There are many different types of epilepsies, and they are called ‘epilepsy syndromes’. An epilepsy syndrome is a collection of signs and symptoms that tend to happen together.
Many children have identifiable epilepsy syndrome, e.g. CAE (Childhood Absence Epilepsy), SeLECTS (Self Limited Epilepsy with Centrotemporal Spikes), or JME (Juvenile Myoclonic Epilepsy). It is important to have a epilepsy syndromic diagnosis, as it may guide individualised management and prognosis.
The following diagram illustrates all the epilepsy syndromes (however, it is very complex!):
What Causes Epilepsy?
The exact cause of Epilepsy can vary and may not always be known. However, several factors or causes can contribute to the development of Epilepsy, such as structural, metabolic, infectious, immunological, genetic causes, or a combination of the above causes.
For example:
- Structural cause – Brain malformation or neuronal migration defect, such as Lisencephaly, Tuberous sclerosis, or Brain Tumours.
- Metabolic cause – Glucose transporter deficiency syndrome (GLUT1 DS)
- Infectious cause – Congenital infections, or meningoencephalitis
- Genetic cause – Chromosomal abnormalities.
What Are The Common Co-Occurring Conditions?
Children with Epilepsy may experience a variety of co-occurring conditions that can impact their overall health and well-being. Some common co-occurring conditions include:
Learning Disability & Neurodevelopmental Disorders
Children with epilepsy may have mild, moderate or severe learning disability. The current research evidence supports that the underlying cause of epilepsy may impact on neurodevelopment. Hence, children and young people with epilepsy may also have neurodevelopment disorders such as cognitive impairments, attention deficit hyperactivity disorder (ADHD) and autistic spectrum disorder (ASD), and conduct problems.
However, some epilepsy syndromes, such as Childhood Absence Epilepsy (CAE) and Self Limited Epilepsy with Centro-temporal Spikes (SeLECTS) are generally not associated with significant neurodevelopment disorders. If a child with one of these epilepsy syndromes experiences significant developmental or learning impairments, an assessment by a paediatric neurologist is indicated.
Behavioural and Emotional Challenges
Living with a long term neurological condition like epilepsy can impact emotional well-being and may contribute to behavioural and psycho-emotional challenges such as anxiety, depression, or social interaction difficulties.
A recent study of children and young adults with epilepsy has shown that 13% had emotional disorder, 7.5% had conduct disorder, and 5% has mixed mental health disorders.
Do children with epilepsy require additional support in school?
It is important that every child with epilepsy should have their educational progress monitored closely so that difficulties can be picked up earlier, and appropriate supports are provided accordingly.
If children with epilepsy have learning difficulties, they may benefit from additional support at school. As learning difficulties can affect their self-esteem and confidence, and in some cases, causing behavioural problems.
How to diagnose Epilepsy?
Diagnosing epileptic seizures and epilepsy in children involves a thorough evaluation by a paediatric neurologist, including medical history, physical examination, developmental assessment, and neurological evaluation.
During your appointment, Dr Yeo will want to know as much as possible about what had happened to your child during the seizures.
It will help Dr Yeo by providing the following information:
- Diary of your child’s seizures (dates, times, description of what had happened before/during/ after the seizures)
- Video recording of your child’s seizures (if possible)
- Bring along the individual who had witnessed your child’s seizures or get a written description from the individual who had witnessed your child’s seizures would be very helpful!
Dr Yeo may suggest the following tests to help with the diagnosis and management of epilepsy:
- Electrocardiogram (ECG): This is a test to check your child’s heart rhythm. This is an essential test to rule out any cardiac conditions that can cause symptoms resembling an epileptic seizure.
- Electroencephalogram (EEG) : This is a brain-wave recording which involves applying quite a few sticky sensors on your child’s head. This is a painless procedure.
- Magnetic Resonance Imaging (MRI) of the brain: These are detailed pictures of the brain to evaluate the structure of your child’s brain.
- Comprehensive neurometabolic testing and/ or genetic testing may be offered to identify underlying metabolic or genetic causes.
Early diagnosis and appropriate treatments are crucial for optimising long term neuro-developmental outcomes and providing appropriate support for children with epilepsy and their families.
How do we treat Epilepsy or Epileptic Seizures? What are Anti-seizure medications?
Once epilepsy is diagnosed in your child, Dr. Yeo will work with you to create a personalised treatment plan. This plan will take into account all aspects of your child’s lifestyle and situation, as well as your family’s preferences.
Dr. Yeo will also collaborate with you and your child to create a Seizure Action Plan, which is a critical plan to follow when a seizure occurs. This plan will include vital information about your child’s medical history, epilepsy syndrome, seizure type, emergency medication plan, and other important details that will help keep your child safe during a seizure.
After considering all of these aspects, Dr. Yeo will guide you and your child in finding the right treatment:
Anti-seizure medication (ASM)
Taking oral medication, i.e. Anti-seizure medication (ASM) to prevent or reduce epileptic seizures and therefore to enhance overall quality of life, is the main treatment for epilepsy.
ASM works by modulating or stabilising the abnormal electrical signals of the brain cells. Considering all aspects, Dr Yeo will guide you and your child finding the right ASM.
Dr Yeo will discuss with you about which ASM have been found to work well, or not work well, for your child’s particular epilepsy, and also the pros and cons of each ASM or other treatment options.
There are other treatment options which may be suggested if they are appropriate:
Ketogenic Diet
The ketogenic diet is a specialist medical diet which contains higher in fats and lower in carbohydrates than a typical diet. This therapy has been known to improve refractory or difficult to control epilepsy, and certain type of epilepsy.
Vagal Nerve Stimulation (VNS)
VNS can be considered for refractory or difficult to control epilepsy. VNS therapy involves implanting a device (i.e. a generator) under the skin of the chest, and wires connecting the device to a nerve in the neck called vagus nerve. The device modulates the electrical signals of the vagus nerve which travels to the brain.
Epilepsy Surgery
Depending on the type of refractory epileptic seizures, epilepsy brain surgery is sometimes offered. There are many types of epilepsy brain surgery, such as focal resection, corpus callosotomy, and hemispherectomy.
What are the Safety Considerations for Children with Epilepsy?
Most children and young people with epilepsy are restricted in their activities; generally because of fear of injury or life threatening event should a seizure occur.
The general advice should be to encourage normal activities as much as possible and to minimise risks by taking common sense precautions. Risk assessment should be individualised for your child.
These are the most high risk situations (‘WHAT’):
- Water activities, e.g. swimming
- Heat, e.g. cooking
- Activities involving heights, e.g. rock climbing
- Traffic, e.g. driving a car, bicycling
References
Dr Yeo is the Course Director of BPNA (British Paediatric Neurology Association) Paediatric Epilepsy Training (PET) for Singapore & South East Asia region.
Dr Yeo’s recent peer-group review journal publications and relevant articles regarding Epileptic Seizures & Epilepsy:
Yoon S, Goh H, Foo CP, Kao MIM, Hie SL, Chan SL, Krishnappa J, Ngoh ASF, Ling SR, Yeo TH, Chan DWS. Parents’ priorities for decision-making of pediatric epilepsy treatments and perceived needs for decision support in multi-ethnic Asian clinical setting: a qualitative analysis. Epilepsy Behav. 2022 Oct;135:108880.
Kumar P, Lim A, HAzrirah SN, ChuaCJH, Ngoh A, Poh SL, Yeo TH, Lim J, Ling S, Sutamam NB, Petretto E, Low DCY, Zeng L, Tan EK, Archachaisri T, Yeo JG, Ginhoux F, Chan D, Alabni S. Single-cell transcriptomics and surface epitope detection in human brain epileptic lesions identifies pro-inflammatory signaling. Nat Neurosci. 2022 Jul;25(7):956-966.
Rr P, Douch C, Aan Koh MJ, Lai AHM, Lim CT, Hartley L, Thomas T, Yeo TH. Speckled brain lesions in Incontinentia Pigmenti patients with acquired brain syndromes. Eur J Paediatr Neurol. 2021 Jul; 33:106-111.
Krishnappa J, Ngoh A, Hong YT, ChunLiang C, Derrick CWS. Unique Severe HyperEkplexia-Like Apneic Events (SHELAE) Improved by High-Dose Piracetam. Child Neurology Open. January 2021.
Hamilton R, Yeo TH, et al. Sensitivity and specificity of the light-adapted ERG in suspected neuronal ceroid lipofuscinoses (NCLs). 54th International Society for Clinical Electrophysiology of Vision Symposium; Aug 13–18, 2016; Singapore. Documenta Ophthalmologica 133 (1S); 35–36. DOI 10.1007/s10633-016-9548-8