Autoimmune Encephalopathy: An important cause of Central Nervous System Inflammation
An increasing number of inflammatory neurological disorders in children are being shown to have a link with our immune system.
Understanding inflammation of central nervous system, such as autoimmune encephalitis, in children is essential for recognising symptoms early and ensuring timely intervention. Delayed recognition and treatment of inflammation of central nervous system can lead to serious health consequences. By learning more about autoimmune encephalitis in children, parents and caregivers can be better equipped to recognise warning signs and seek appropriate medical care.
What is Autoimmune encephalitis?
- Encephalitis means inflammation of the brain tissue.
- Encephalitis may initially present with flu-like symptoms such as fever, general lethargy or headache.
- These flu-like symptoms can become more severe in some cases, which can lead to confusion, drowsiness, seizures or problems with breathing and heart muscle function.
- Encephalitis can be caused either by an infection invading the brain (infectious encephalitis, eg. Herpes Simplex Virus Encephalitis) or through the immune system attacking the brain (such as Autoimmune Encephalitis)
What are the common types of Autoimmune Encephalitis?
- Acute Disseminated Encephalomyelitis (ADEM)
- Anti-N-Methyl-D-Aspartate (anti-NMDA) receptor encephalitis
- Limbic Encephalitis
- Hashimoto Encephalopathy
- Rasmussen Encephalitis
What are the important signs and symptoms of encephalitis?
Common presentation:
- Sudden or acute change
- Preceding flu-like illness with headache and fever
- Altered consciousness
- Lethargy/ drowsiness
- Behavioural changes, such as agitation
- With or without seizures
- Abnormal movement
- Hallucinations
- Sleep disturbance
- Speech impairment
- Presentation can be subtle and fluctuant
How is anti-NMDAR autoimmune encephalitis in Children Diagnosed?
Diagnosing Anti-NMDR autoimmune encephalitis in children can be challenging, and it involves a thorough evaluation by a paediatric neurologist, including a detailed medical history, physical examination, neurological assessment, and neuroimaging, such as MRI brain scan.
A procedure called lumbar puncture (spinal tap) will be carried out to check for signs of infection in the brain or spinal cord. The blood and fluid collected from the lumbar puncture (LP) – Cerebrospinal Fluid (CSF) will be analysed for the DNA fragments of important and common viruses, such as HSV, VZV (chickenpox), Enteroviruses. Blood and CSF will be analysed for inflammatory markers, and specific antibodies, including NMDAR.
MRI brain is recommended as it is more sensitive in picking up abnormal changes than CT head. Electroencephalogram (EEG) tests maybe requested to analyse your child’s brain wave signals/ pattern.
Early detection and treatment are critical for optimising clinical outcomes and providing appropriate support for affected children and families.
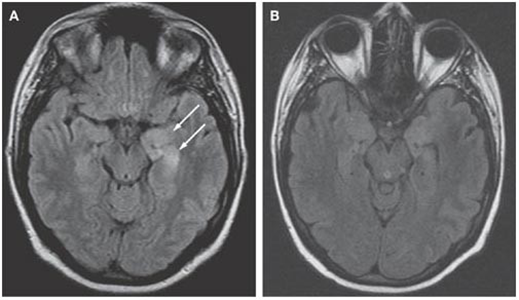
ansing, L., Tüzün, E., Ko, M. et al. A patient with encephalitis associated with NMDA receptor antibodies. Nat Rev Neurol 3, 291–296 (2007). https://doi.org/10.1038/ncpneuro0493
Why encephalitis is missed in children or adults?
- Wrongly attributed a child’s fever and confusion to an urinary tract infection (based on urine dipstick) or chest infection (based on a few chest signs), without strong evidence.
- Failure to realised that a child has a febrile illness, just because they are not febrile during assessment.
- Ignoring a caregiver’s complaint that a child is ‘not quite right’, sleepy, or lethargic.
- Wrongly attributing clouding of consciousness to drugs or alcohol, without good evidence.
- Failure to properly investigate a child with a fever and seizure, following which they do not recover consciousness
- Failure to do a lumbar puncture even though there are no contraindications.
What is the treatment for Anti-NMDAR autoimmune encephalitis in Children?
Treatment for children with Anti-NMDAR autoimmune encephalitis aim to manage symptoms, and to improve long-term outcomes by dampening down the over-active immune system.
Medication
Anti-viral and antibiotic, such as intravenous Aciclovir and Ceftriaxone, should be started after lumbar puncture, or if CSF is consistent with viral encephalitis. If lumbar puncture is not possible, it is important to start anti-viral and antibiotics anyway, especially if brain scan is consistent with viral encephalitis, or there is a strong clinical suspicion. Anti-viral and antibiotics can then be stopped if the initial investigations are negative for infections.
Medications may be prescribed to manage symptoms. For example, anti-seizure medications may help control seizures, and oral clonidine or lorazepam may help tackle behaviour disturbance and agitation.
High dose intravenous steroids and/ or intravenous immunoglobulin (IVIGG) are recommended treatment to modulate and also to dampen down the over-active immune system. In severe cases, plasma exchange may be recommended.
Around 20% of children with Autoimmune encephalopathy, such as NMDAR autoimmune encephalopathy, can have relapse of their symptoms. Hence, other immunosuppressive therapy such as Rituximab or mycophenolate mofetil (MMF) may be recommended.
Rehabilitation Therapy
Rehabilitation therapy, including physical therapy, occupational therapy, speech therapy, music therapist, and orthotist plays a crucial role in helping children recover and regain function after brain infection or inflammation. These therapies improve mobility, motor skills, communication, and daily living activities; Appropriate equipments or aids, and orthotic devices can be useful in improving mobility and posture.
Supportive Care
Supportive care measures, including close monitoring, hydration, nutrition support, and management of other medical conditions, are essential for optimising outcomes and preventing complications in children with CNS infections and/ or inflammation.
Long-Term Follow-Up
Long-term follow-up with a paediatric neurologist and allied healthcare providers are essential to monitor the child’s progress, adjust treatment as needed, and address any new or ongoing concerns. Regular evaluations may include imaging studies, neurological assessments, and developmental screenings may be used to track the child’s recovery and outcome measures.
Most children with autoimmune encephalitis make a good neurological recovery. However, this may take months rather than weeks. Seizures and motor abilities are the symptoms that tend to recover first. Additional supports in school may be needed as some children may continue to have behavioural and/ or cognitive difficulties for longer period of time. Recovery may take up to two years.
References
Dr Yeo’s recent peer-group review journal publications and abstracts regarding infections and inflammation of Central Nervous System:
Kumar, Pavanish & Lim, Amanda & Hazirah, Sharifah & Chua, Camillus & Ngoh, Adeline & Poh, Su Li & Yeo, Tong & Lim, Jocelyn & Ling, Simon & Sutamam, Nursyuhadah & Petretto, Enrico & Low, David & Zeng, Li & Tan, Eng-King & Arkachaisri, Thaschawee & Yeo, Joo & Ginhoux, Florent & Chan, Derrick & Albani, Salvatore. (2022). Single-cell transcriptomics and surface epitope detection in human brain epileptic lesions identifies pro-inflammatory signaling. Nature Neuroscience. 25. 1-11. 10.1038/s41593-022-01095-5.
Rr, Pravin & Douch, Catherine & Koh, Mark & Lai, Angeline & Lim, Tchoyoson & Hartley, Louise & Thomas, Terrence & Yeo, Tong. (2021). Speckled brain lesions in Incontinentia Pigmenti patients with acquired brain syndromes. European Journal of Paediatric Neurology. 33. 10.1016/j.ejpn.2021.05.012.
Yeo TH, Vassallo G, Judge M, Laycock N, Kelsey A, Crow YJ. Infantile neurological Degos disease. Eur J Paediatr Neurol. 2011 Mar;15(2):167-70.